|

Vaginal discharge during Chlamydia could be noted only in 25-30% cases. Most typical for Chlamydia is abnormal vaginal discharge (mucus or pus), smelling yellowish discharge from the cervix - both combined with frequent urges to urinate (much more than usual).
|
Chlamydia is a common sexually transmitted disease (STDs) caused by the bacterium, Chlamydia trachomatis, which can damage a woman's reproductive organs. Even though symptoms of Chlamydia are usually mild or absent - serious complications that cause irreversible damage, including infertility, can occur "silently" before a woman ever recognizes a problem.
Chlamydia is one of the most common sexually transmitted diseases. The Centers for Diseases Control and Prevention (CDC) estimates that more than 3 million cases of Chlamydia occur every year. CDC estimates that a staggering four to eight million new cases occur each year. As the infection frequently causes no symptoms, the number of infected people could be 4 times higher.
The highest rates of Chlamydia are noted among youth – 15-19 year olds.
CHLAMYDIA transmission
Chlamydia can be transmitted during vaginal, anal, or oral sex. Chlamydia can also be passed from an infected mother to her baby during vaginal childbirth (with subsequent neonatal eye infection or pneumonia). Chlamydia can also lead to premature birth or low birth weight.
Any sexually active person can be infected with Chlamydia. Multiple sexual partners are increasing the risk for Chlamydia transmission. The greater the number of sex partners, the greater the risk of infection. Higher is the risk for Chlamydia transmission in youth – teenagers and young women - because the cervix (opening to the uterus) of teenage girls and young women is not fully matured and is probably more susceptible to infection, they are at particularly high risk for infection if sexually active.
The bacteria can infect the throat from oral sexual contact with an infected partner. It can also cause an inflamed rectum and inflammation of the lining of the eye (“pink eye”).
CHLAMYDIA symptoms
Approximately 75% women who have Chlamydia have no symptoms. About 25% women with Chlamydia could mention all typical symptoms - if Chlamydia symptoms do occur, they usually appear within 1 to 3 weeks after infection exposure and/or transmission. Very often Chlamydia is called "silent" disease because the majority of infected people have no symptoms. In women, the bacteria initially infect the cervix and the urethra (urine canal). Chlamydia infection of the cervix can spread to the rectum.
|
|
Chlamydia symptoms include:
- abnormal vaginal discharge (mucus or pus),
- smelling yellowish discharge from the cervix,
- frequent urges to urinate (much more than usual),
-
burning sensation or pain during urination,
- abdominal and/or low back pain,
- nausea,
- fever (often low-grade fever),
-
pain during intercourse,
-
vaginal bleeding between periods,
- vaginal bleeding after sex,
- eye infections (conjunctivitis).
Women who have receptive anal intercourse may acquire Chlamydia infection in the rectum, which can cause rectal pain, discharge, or bleeding. If the anus is infected, women may have rectal pain or tenderness and a yellow discharge of pus and mucus from the rectum.
|
Chlamydia genital infections occasionally cause a joint inflammation called reactive arthritis. Reactive arthritis typically affects several joints at once. The lower limbs are affected most often. The inflammation seems to be an immune reaction to the genital infection rather than spread of the infection to the joints.
Chlamydia can also be found in the throats of women after having oral sex with an infected partner.
CHLAMYDIA complications
 Chlamydia can be easily treated and cured but if untreated, Chlamydia infection can progress to serious reproductive and other health problems with both short-term and long-term consequences. Like the disease itself, the damage that Chlamydia causes is often "silent." Chlamydia can be easily treated and cured but if untreated, Chlamydia infection can progress to serious reproductive and other health problems with both short-term and long-term consequences. Like the disease itself, the damage that Chlamydia causes is often "silent."
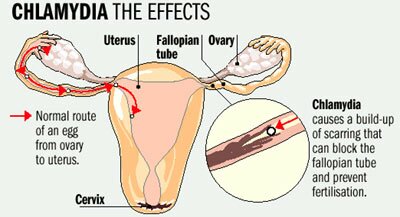
 In women, untreated Chlamydia infection can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease (PID). This happens in about 10-15% of women with untreated Chlamydia. Each year, approximately 500,000 women in the United States develop PID due to Chlamydia infections. In women, untreated Chlamydia infection can spread into the uterus or fallopian tubes and cause pelvic inflammatory disease (PID). This happens in about 10-15% of women with untreated Chlamydia. Each year, approximately 500,000 women in the United States develop PID due to Chlamydia infections.
 Chlamydia can also cause fallopian tube infection without any symptoms. PID and “silent” infection in the upper genital tract can cause permanent damage to the fallopian tubes, uterus, and surrounding tissues. The damage can lead to chronic pelvic pain, infertility, miscarriage and increased risk of potentially fatal ectopic pregnancy. It is important to mention that Chlamydia could also increase the chances of becoming infected with HIV, if exposed. Chlamydia can also cause fallopian tube infection without any symptoms. PID and “silent” infection in the upper genital tract can cause permanent damage to the fallopian tubes, uterus, and surrounding tissues. The damage can lead to chronic pelvic pain, infertility, miscarriage and increased risk of potentially fatal ectopic pregnancy. It is important to mention that Chlamydia could also increase the chances of becoming infected with HIV, if exposed.
 |
 To help prevent the serious consequences of Chlamydia sexually transmitted infection, screening at least annually for Chlamydia is recommended for all sexually active young women (15-25 year old). The annual screening test for Chlamydia is also recommended for older women with risk factors for Chlamydia (new sex partner or multiple sex partners). Chlamydia test is very important for pregnant women because Chlamydia can lead to premature birth or low birth weight. Chlamydia can also be passed from an infected mother to her baby during vaginal childbirth (with subsequent neonatal eye infection or pneumonia). To help prevent the serious consequences of Chlamydia sexually transmitted infection, screening at least annually for Chlamydia is recommended for all sexually active young women (15-25 year old). The annual screening test for Chlamydia is also recommended for older women with risk factors for Chlamydia (new sex partner or multiple sex partners). Chlamydia test is very important for pregnant women because Chlamydia can lead to premature birth or low birth weight. Chlamydia can also be passed from an infected mother to her baby during vaginal childbirth (with subsequent neonatal eye infection or pneumonia).
 Rarely, genital Chlamydia infection can cause arthritis that can be accompanied by skin lesions and inflammation of the eye and urethra (Reiter's syndrome). Rarely, genital Chlamydia infection can cause arthritis that can be accompanied by skin lesions and inflammation of the eye and urethra (Reiter's syndrome).
CHLAMYDIA and pregnancy
In pregnant women, there is some evidence that untreated Chlamydia infections can lead to premature delivery and/or or low birth weight. Babies who are born to infected mothers can get Chlamydia infections in their eyes and respiratory tracts. Chlamydia is a leading cause of early infant pneumonia and conjunctivitis (pink eye) in newborns.
CHLAMYDIA – how to discover
Laboratory tests can easily diagnose Chlamydia infection. Chlamydia tests can be performed on urine and/or on specimen collected from vagina and/or cervix.
It is recommended to combine the Chlamydia test with gonorrhea test (at the same time) because sometimes both sexes have gonorrhea and Chlamydia infection at the same time.
Gonorrhea, which is often also present, can be diagnosed from the same sample. Specific tests for genital infections with Ureaplasma and mycoplasmas are not usually done. These infections are sometimes diagnosed in people with characteristic symptoms after gonorrhea and Chlamydia infections are ruled out.
As Chlamydia infection is so common and because many infected women have no symptoms, the annual Chlamydia tests are recommended for sexually active young women (15-25 year old) – as a part of STD screening.
CHLAMYDIA treatment
Chlamydia can be easily treated and cured with antibiotics. Treatment can consist of a single dose of an antibiotic or a week's worth of antibiotic twice daily. A single dose of azithromycin or one week of doxycycline (twice daily) are the most commonly used treatments. During treatment, sexual activity should not occur.
All sex partners should be evaluated, tested and treated. Persons with Chlamydia should abstain from sexual intercourse until they and their sex partners have completed treatment, otherwise re-infection is possible.
Women whose sex partners have not been appropriately treated are at high risk for re-infection. Having multiple infections increases a woman's risk of serious reproductive health complications, including infertility. Retesting should be encouraged three months after treatment of an initial infection. This is especially true if a woman does not know if her sex partner received treatment.
|
BE CAREFUL
If left untreated Chlamydia can cause permanent damage to the reproductive system and develop infertility. Remember - the damage that the untreated Chlamydia causes may go unnoticed because often there are no symptoms. Chlamydia is known as “silent” STD. Chlamydia treatment should be done properly even you don’t have symptoms.
|
It is important to mention that both partners with Chlamydia must be treated at the same time to prevent re-infection. Antibiotics such as doxycycline, tetracycline, and Zithromax are all effective against Chlamydia. Erythromycin is often prescribed for pregnant women and others who cannot take tetracycline.
If Chlamydia urethritis is not treated, symptoms usually disappear in 4 to 6 weeks. However, if untreated, the Chlamydia infection can cause several serious complications, especially in women who have been infected a long time.
The risk of another Chlamydia infection or another STD within 3 to 4 months is high enough that people should be screened again at that time.
CHLAMYDIA prevention
 The surest way to avoid transmission of STDs is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected. The surest way to avoid transmission of STDs is to abstain from sexual contact, or to be in a long-term mutually monogamous relationship with a partner who has been tested and is known to be uninfected.
 Latex male condoms, when used consistently and correctly, can reduce the risk of transmission of Chlamydia. Latex male condoms, when used consistently and correctly, can reduce the risk of transmission of Chlamydia.
 It is recommended yearly Chlamydia testing of all sexually active young women (15-25 year old). Regular Chlamydia tests are also recommended for older women with risk factors for Chlamydia infections (those who have a new sex partner or multiple sex partners), and for all pregnant women. An appropriate sexual risk assessment by a health care provider should always be conducted and may indicate more frequent screening for some women. It is recommended yearly Chlamydia testing of all sexually active young women (15-25 year old). Regular Chlamydia tests are also recommended for older women with risk factors for Chlamydia infections (those who have a new sex partner or multiple sex partners), and for all pregnant women. An appropriate sexual risk assessment by a health care provider should always be conducted and may indicate more frequent screening for some women.
|
Important to Know
Women and teenage girls should be re-tested a few months after treatment - because of the risk of re-infection from an untreated partner. Chlamydia can make hard not-reversible damage to the reproductive system. It is important to make sure the Chlamydia has been treated completely and that re-infection has not occurred.
|
 Any genital symptoms such as an unusual sore, discharge with odor, burning during urination, or bleeding between menstrual cycles could mean an STD infection. If a woman has any of these symptoms, she should stop having sex and consult a health care provider immediately. Treating STDs early can prevent PID. Women who are told they have an STD and are treated for it should notify all of their recent sex partners (sex partners within the preceding 60 days). Sexual activity should not resume until all sex partners have been examined and, if necessary, treated. Any genital symptoms such as an unusual sore, discharge with odor, burning during urination, or bleeding between menstrual cycles could mean an STD infection. If a woman has any of these symptoms, she should stop having sex and consult a health care provider immediately. Treating STDs early can prevent PID. Women who are told they have an STD and are treated for it should notify all of their recent sex partners (sex partners within the preceding 60 days). Sexual activity should not resume until all sex partners have been examined and, if necessary, treated.
|